Summary
Bone marker tests measure substances in the blood and urine that are produced as bones remodel themselves as part of the natural regeneration cycle.
They are used to evaluate and monitor the rate of bone resorption and formation. They can help in the diagnosis of age-related bone loss conditions such as osteoporosis as well as disorders such as Paget’s disease, osteomalacia, cancer, hyperparathyroidism, hypothyroidism, chronic kidney failure and Cushing’s syndrome.
They are also useful in monitoring the effectiveness of treatment. However, they are not diagnostic and cannot show the cause of a health problem. They offer additional information to the doctor but do not take the place of bone mineral density screening.
Bone marker tests measure substances in the blood and urine that are produced as bones remodel themselves as part of the natural regeneration cycle.
They are used to evaluate and monitor the rate of bone resorption and formation. They can help in the diagnosis of age-related bone loss conditions such as osteoporosis as well as disorders such as Paget’s disease, osteomalacia, cancer, hyperparathyroidism, hypothyroidism, chronic kidney failure and Cushing’s syndrome.
They are also useful in monitoring the effectiveness of treatment. However, they are not diagnostic and cannot show the cause of a health problem. They offer additional information to the doctor but do not take the place of bone mineral density screening.
Why get tested?
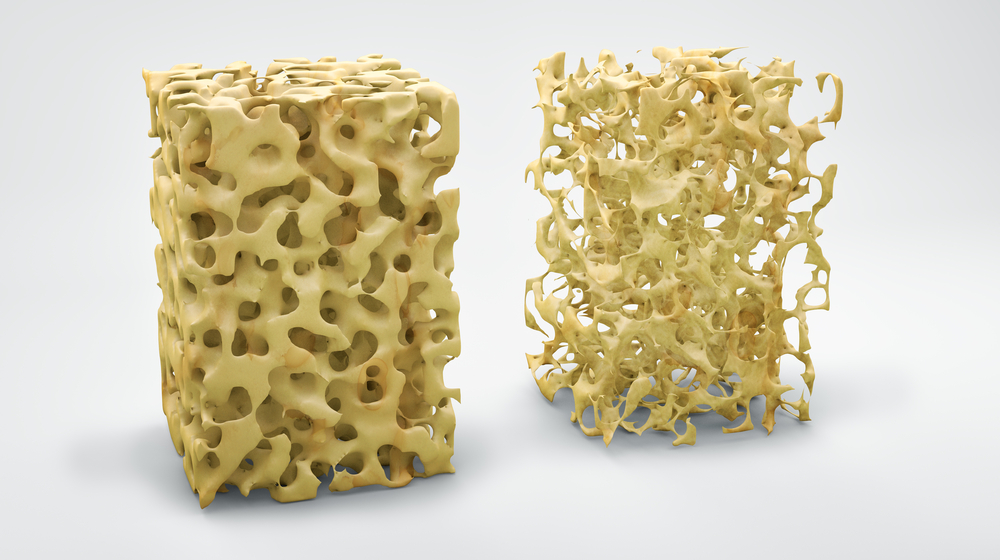
Bone is a living, growing tissue that is constantly rebuilding itself replacing old weak bone with new fresh bone tissue. To do this the body breaks down and dissolves old bone into minerals and collagen and then resorbs this while at the same time growing new bone. In order to keep bones healthy it is important that the amount of bone that is removed is replaced with the same amount of new bone. In young, healthy people the amount of bone removed is about the same as that replaced but as we age the process becomes unbalanced and there can be a loss of bone structure and strength, which leads to bone disorders such as osteoporosis.
Bone is made up largely of type-I collagen, a protein network that gives the bone its strength, and calcium phosphate. There are two major types of cells in bone: osteoblasts and osteoclasts. Osteoblasts are the cells that lay down new bone but they first initiate bone resorption by stimulating osteoclasts, which digest small amounts of bone in the area that needs strengthening. To do this they use acid and enzymes to dissolve the protein network. Osteoblasts then initiate new bone formation by releasing a variety of substances that help form a new protein network which is then mineralised with calcium and phosphate.
This on-going remodelling process takes place on a microscopic scale throughout the body to keep bones alive and sturdy. During early childhood and in the teenage years new bone is added faster than old bone is removed. People generally reach their peak bone mass (maximum bone density and strength) between the ages of 25 and 30. The age at which someone begins to experience symptoms of bone loss depends on the amount of bone that was developed during their youth and the rate of bone resorption.
As well as ageing, several diseases and conditions can cause an imbalance between bone resorption and formation. These include rheumatoid arthritis, hyperparathyroidism, Cushing disease, chronic kidney disease, multiple myeloma, as well as prolonged use of drugs such as antiepileptics, glucocorticoids, or lithium.
Bone markers measure substances that are released into the blood and urine during bone resorption and rebuilding. They are enzymes or other proteins associated with the breakdown and resorption process or else the formation of collagen. They can be useful in detecting the imbalance and bone loss.Two blood tests are recommended for evaluating bone turnover:
Other bone marker tests that may sometimes be used include:
Bone marker testing is often performed along with other tests such as a calcium, vitamin D, thyroid testing, and parathyroid hormone when bone loss is detected during a bone mineral density test (diagnostic imaging) and/or when a person has a history of unexpected bone fracture. One or more bone marker tests can sometimes be used before anti-resorptive or bone formation therapy and then typically three to six months later to monitor the effectiveness of treatment. They can be helpful in deciding if the dose of the drug a person is receiving is effective.
Typically no one will have all of the tests done that are described here. Most doctors use one or a few particular bone markers to evaluate bone resorption and bone formation. The choice of bone markers will depend on many factors, including your medical history, signs and symptoms, and physical examination, and these all vary from person to person. In general if a test is ordered as a baseline prior to therapy, then the same test will be ordered later so that the two results can be compared.
Bone marker testing is typically only indicated in those people who have been diagnosed with or are at risk of bone loss. The tests are not intended to be used to screen the general public. They offer additional information to the doctor but do not take the place of bone mineral density screening.
Having the test
Sample
Blood or urine
Any preparation?
Fasting may be required before testing and samples are typically collected in the morning. Many of the bone markers in the blood and urine vary in concentrations depending on the time of day (diurnal variation), so sample timing can be important. Carefully follow any instructions given for the timing of sample collection. For example, you may be asked to collect urine from the second time you pass urine in the morning (a second morning void).
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
Reference intervals
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation.
Your results need to be interpreted by your doctor. Concentrations of bone markers are affected by many factors, particularly during childhood development. These include age, sex, growth velocity, nutritional status, and puberty. A high level of one or more bone markers in urine and/or blood suggests an increased rate of resorption and/or formation of bone, but it does not indicate the cause. You will probably need other tests to learn more about your condition.
High levels of bone markers may be seen in conditions such as:
- Osteoporosis
- Paget’s disease
- Cancer that has spread to the bone (metastatic bone disease)
- Hyperparathyroidism
- Hyperthyroidism
- Osteomalacia in adults and rickets in children—lack of bone mineralisation, often due to vitamin D or calcium deficiency
- Chronic kidney failure (renal osteodystrophy)
- Excess use or high doses of glucocorticoids or Cushing’s syndrome
A low or normal level suggests no excessive bone turnover.
When used to monitor anti-resorptive therapy, decreasing levels of the bone resorption markers over time reflect a response to therapy
Questions to ask your doctor
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Any more to know?
People can and should take steps to maintain bone health throughout their life, but bone markers themselves are not affected by lifestyle changes. If you have bone loss, work with your healthcare practitioner to determine the best treatment for you.
More information
Pathology and diagnostic imaging reports can be added to your My Health Record. You and your healthcare provider can now access your results whenever and wherever needed.
Get further trustworthy health information and advice from healthdirect.
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.