What is being tested?
Lupus anticoagulant is a protein that increases the risk of developing blood clots in both the veins and arteries. These clots may block blood flow in any part of the body, leading to strokes, heart attacks, pulmonary embolisms, deep vein thrombosis, and to recurrent foetal loss, especially in the 2nd and 3rd trimesters (thought to be related to clotting in placental blood vessels). The lupus anticoagulant is an acquired, not inherited, condition. Although it is found most frequently in those with autoimmune diseases, such as systemic lupus erythematosus (SLE), the lupus anticoagulant may also be seen chronically or temporarily in those with infections or cancers and in those who are taking certain medications, such as phenothiazines, chlorpromazine, procainamide and fansidar. It is thought to be present in about 1 – 2% of the general population, and may develop in people with no known risk factors.
The term lupus anticoagulant (LA) is misleading. It is not a diagnostic test for lupus but gets its name because it was first discovered in patients with SLE, and because it often prolongs the activated partial thromboplastin time (APTT) test - a timed blood test usually associated with anticoagulation and bleeding, not with thrombosis. It prolongs the APTT test, as well as several other related tests, because the lupus anticoagulant binds to phospholipids and the reagents (chemicals) used in performing the APTT test contain phospholipids.
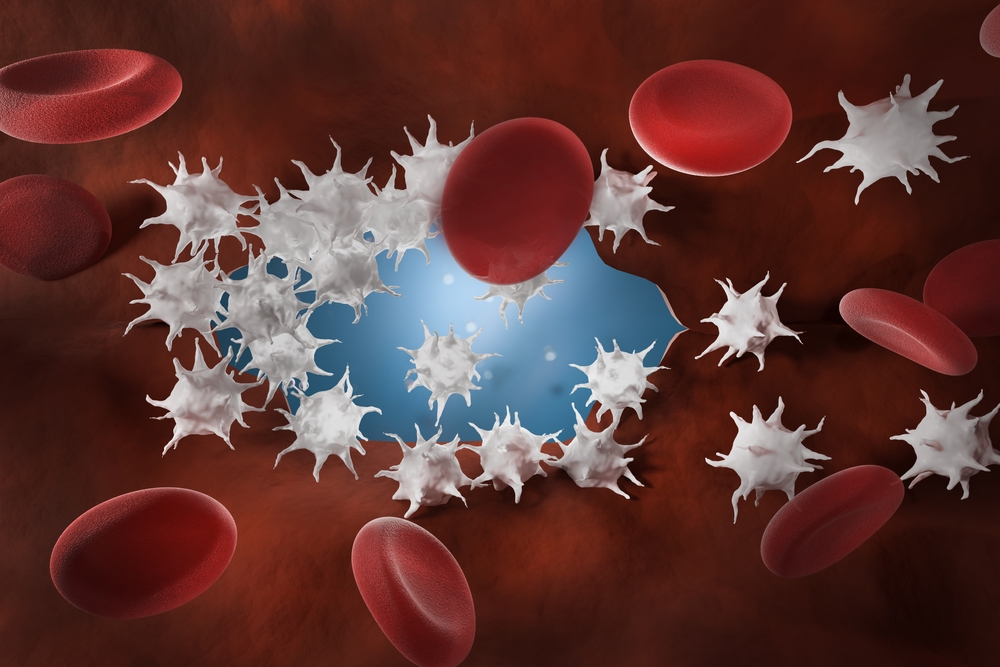
In the body phospholipids play a vital role in the blood clotting process. They are found primarily on the surface of platelets and cell membranes and assist in the activation of several coagulation factors - proteins that are sequentially activated in response to blood vessel or tissue damage in a process called the coagulation cascade.
The lupus anticoagulant is one of three types of test for antiphospholipid syndrome, associated with an increased risk of thrombosis. The others are anticardiolipin antibodies and antibodies against beta-2 glycoprotein 1 (less common). Any or all may be positive in antiphospholipid syndrome (also called Hughes' syndrome). Each interferes with the clotting process in a fashion that is not well understood and, singly or together, they increase a person's tendency to clot.
While anticardiolipin and anti-beta-2 glycoprotein 1 antibodies may be tested for directly, there is not a single test for the lupus anticoagulant. It is usually diagnosed by using a panel of sequential tests that are taken through different stages. These tests operate on the principle that the lupus anticoagulant is a non-specific inhibitor – it does not target a specific coagulation factor, it binds to the assay’s phospholipids, inhibiting and prolonging the tests.
The first test is usually an APTT (or an LA-APTT, a version of the test made more sensitive to LA) and the first stage is to see whether the original test is prolonged. If it is, then the patient’s plasma is mixed with pooled normal plasma (a combination of blood from different donors that contains all of the coagulation factors). If the prolongation is due to a specific coagulation factor deficiency then the normal plasma should "correct" the test to normal. If it is due to a non-specific inhibitor it will still be prolonged. In the third stage, additional phospholipids are added to the test. This should be sufficient to correct the test to near normal levels if the lupus anticoagulant is the cause of the abnormality. The dilute Russell Viper venom test is a sensitive APTT-like test for LA, and can also be performed with a phospholipid correction step.
How is it used?
Lupus anticoagulant testing is used to help determine the cause of an unexplained thrombosis, recurrent fetal loss, or a prolonged APTT test. It is used to help determine whether a prolonged APTT is due to a specific inhibitor (an antibody against a specific coagulation factor) or to a non-specific inhibitor, like the lupus anticoagulant. It may be used with anti-cardiolipin antibody and anti-beta-2 glycoprotein 1 antibodies assay to check for the presence of antiphospholipid syndrome. If someone tests positive for the lupus anticoagulant, the test may be done again in several weeks to see if the antibody was due to a temporary condition or is a chronic issue. Occasionally lupus anticoagulant testing may be ordered to help determine the cause of a positive VDRL/RPR test for syphilis (both anticardiolipin and lupus antibodies will test false positive with these tests).
Because there are other inhibitors and analytical variables that can cause abnormal test results, several different tests are used to confirm the presence of a lupus anticoagulant. Typically these may include: APTT, prothrombin time (PT), dilute or modified Russell viper venom screen (dRVVT or MRVVT), and a hexagonal (II) phase phospholipid assay (Staclot-LA test) or kaolin clot time. A thrombin time test may also be done to rule out heparin contamination (this is a drug used for anticoagulant therapy), and a fibrinogen test may be done to rule out hypofibrinogenaemia. These two conditions can cause prolongations in the test results and interfere with lupus anticoagulant detection.
When is it requested?
Lupus anticoagulant testing is requested when a patient has had an unexplained thrombotic episode, has had recurrent miscarriages, and/or as a follow-up to a prolonged APTT test. If a lupus anticoagulant panel is positive your doctor may want to repeat one or more of the tests several weeks later to determine whether the lupus inhibitor is transitory or chronic.
Your doctor may also want to test for the lupus anticoagulant when you have a positive anticardiolipin antibody, to evaluate whether you have antiphospholipid syndrome.
If you are negative for the lupus anticoagulant but have an autoimmune disease, such as SLE or a mixed connective tissue disorder, your doctor may occasionally request one or more of the lupus anticoagulant screening tests, usually the APTT, to determine whether or not you may have developed the lupus anticoagulant. This is most likely if you have developed symptoms suggestive of blood clot formation, such as pain and swelling in the extremities, shortness of breath, headaches, etc.
What does the result mean?
The results of each of the lupus anticoagulant tests either lead towards or away from the likelihood of having a lupus anticoagulant. Although the tests done may vary, they usually begin with a prolonged APTT.
Other tests that may be done to help confirm the diagnosis of a lupus anticoagulant include:
Other tests that may be run in addition to lupus anticoagulant testing:
Is there anything else I should know?
Patients on heparin or heparin substitute (such as hirudin, danaparoid, or argatroban) anticoagulation therapy may have false positive results for lupus antibodies but those on warfarin (coumadin) anticoagulant therapy should not. If possible, lupus anticoagulant testing should be done prior to the start of anticoagulation therapy. If a patient with a thrombosis has a lupus anticoagulant it may be necessary to prolong and possibly increase the intensity of their anticoagulation therapy.
In addition to testing for lupus antibodies, it may sometimes be necessary to test for coagulation factor VIII levels. Coagulation factor VIII inhibitors (specific antibodies against factor VIII) can decrease factor VIII levels and cause false positive lupus anticoagulant tests. Elevated factor VIII levels, as may be seen in an acute infection or with replacement therapy when someone has Haemophilia A, may shorten the APTT time, leading to a temporary false negative test for lupus anticoagulant.
Common questions
Yes. Besides heparin contamination, other pretest variables may have a significant impact on detecting the lupus anticoagulant. The blood sample is collected in a special citrated tube and centrifuged to remove the plasma (liquid part) for testing. There must be the proper amount of blood in the tube and it cannot be clotted. When the blood is centrifuged most of the platelets are left behind. If there are too many in the plasma sample, it may be compromised (because platelets are a source of phospholipids). Also, if the patient’s haematocrit (the amount of solid components in their blood) is elevated or decreased test results may be affected.
No treatment is required if someone does not have any symptoms. If blood clots do occur, patients are usually anticoagulated with heparin (which is injected under the skin or given intravenously (IV)) followed by oral warfarin (coumadin) therapy for several months. Higher than normal doses of warfarin may be required in this situation and the treatment may need to be continued for a longer period of time than normal. In someone with the lupus anticoagulant the risk of recurrence of both arterial and venous thrombotic episodes is relatively high. Some patients may need to be on long-term (even life-long) oral anticoagulation.
In general, anticardiolipin antibodies are more common than the lupus anticoagulant. Anticardiolipin antibodies occur approximately five times more often than the lupus anticoagulant in patients with the antiphospholipid antibody syndrome. About sixty percent of those with the lupus anticoagulant will also have anticardiolipin antibodies.
More information
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.