What is being tested?
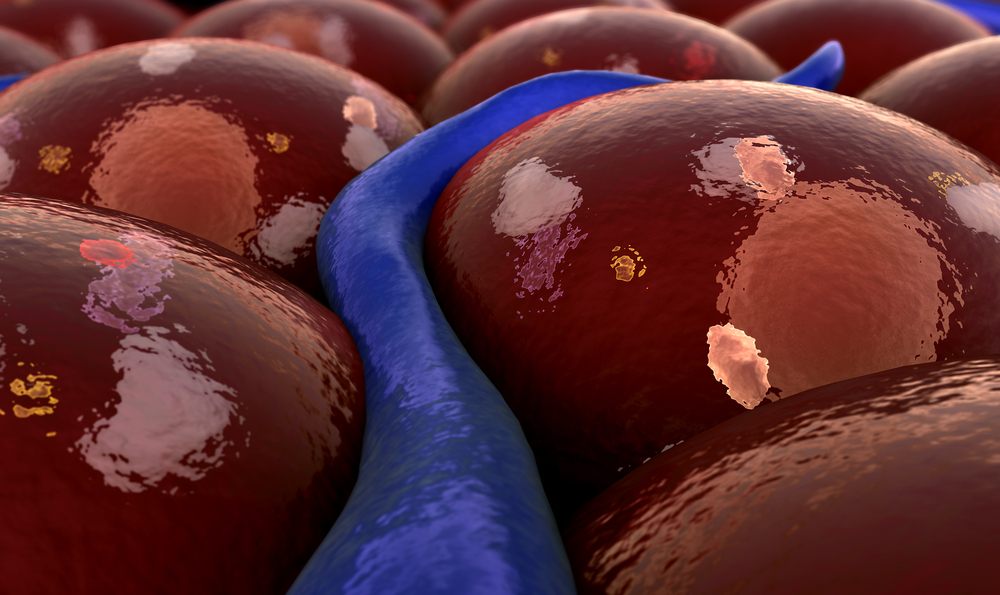
This test detects the presence or absence of human leukocyte antigen B27 (HLA-B27) on the surface of white blood cells in a blood sample. Human leukocyte antigens (HLA) are a group of proteins that help the body's immune system to identify its own cells and to distinguish between 'self' and 'nonself'. Everyone has an inherited combination of HLA antigens present on the surface of his or her white blood cells (leukocytes) and other nucleated (containing a nucleus) cells.
These HLA antigens are divided into types: Class I (A, B, C) and Class II (DR, DP, DQ). While not as unique as a fingerprint, the presence or absence of each antigen creates a distinctive HLA combination for each person.
HLA-B27 is found in about 5-10% of the Australian population. Its presence has been associated with several autoimmune disorders. The most common of these disorders is ankylosing spondylitis (AS). Approximately 90% of patients with AS are positive for HLA-B27. Other disorders that have an association with the presence of HLA-B27 include:
HLA-B27 may also be present in patients with inflammatory bowel disease and with a range of other chronic conditions. While HLA-B27 has not been established as a cause of these disorders, there is a higher prevalence of this antigen in those affected.
How is it used?
The HLA-B27 test is primarily ordered to help strengthen or confirm a suspected diagnosis of ankylosing spondylitis (AS), reactive arthritis or sometimes anterior uveitis. The HLA-B27 test is not a definitive test that can be used to diagnose or rule out a disorder. It is used as one piece of evidence in a constellation of signs, symptoms, and laboratory tests to support or rule out the diagnosis of certain autoimmune disorders, such as ankylosing spondylitis (AS) and reactive arthritis. Both AS and reactive arthritis are chronic, progressive conditions that occur more frequently in men than women, and the first symptoms usually occur when a patient is in his early 30's. Ankylosing spondylitis is characterised by pain, inflammation, and a gradual stiffening of the spine, neck and chest. Reiter's syndrome is a group of symptoms that includes inflammation of the joints, urethra (urethritis), eyes, and skin lesions. Often patients do not have urethritis and so the term reactive arthritis is a better name. Often the initial symptoms of these autoimmune disorders are subtle and may take several years before characteristic degenerative changes to bones and joints are visible on X-rays. Anterior uveitis is associated with recurring inflammation of the structures of one or both eyes.
The HLA-B27 test may be ordered as part of a group of tests used to diagnose and evaluate conditions causing arthritis-like chronic joint pain, stiffness, and inflammation. This group of tests may include an RF (rheumatoid factor) with either an ESR (erythrocyte sedimentation rate) or a CRP (C-reactive protein). HLA-B27 is sometimes ordered to help evaluate someone with recurrent uveitis that is not caused by a recognisable disease process.
When is it requested?
An HLA-B27 test may be ordered when a patient has acute or chronic pain and inflammation in his or her spine, neck, chest, eyes, and/or joints, and the doctor suspects an autoimmune disorder that is associated with the presence of HLA-B27. Doctors frequently must rely on their clinical findings and the HLA-B27 test result when diagnosing ankylosing spondylitis, and other HLA-B27 related disorders, because the characteristic changes to the bones may not be detectible for several years. Under these circumstances, HLA-B27 is not diagnostic but adds additional information, increasing or decreasing the likelihood that the patient has ankylosing spondylitis. An HLA-B27 may also be ordered when a patient has recurrent uveitis.
What does the result mean?
HLA-B27 will be present or absent. If it is present, then the HLA-B27 antigen exists on the surface of the body's white blood cells and other nucleated (containing a nucleus) cells. If a patient has HLA-B27 and has symptoms such as chronic pain, inflammation and/ or degenerative changes to his or her bones (as seen on X-ray), then it supports a diagnosis of AS, reactive arthritis or another autoimmune disorder that is associated with the presence of HLA-B27. This is especially true if the patient is young, male and if he experienced his first symptoms before the age of 40.
If HLA-B27 is not present, then the association is not there. This does not, however, mean that the person does not have the suspected condition, as a certain percentage of patients with each disorder will be HLA-B27 negative.
A positive HLA-B27 in a person who does not have symptoms or a family history of HLA-B27 associated disease is not clinically significant. It does not help predict the likelihood of developing an autoimmune disease. If a patient does have an associated disorder, the presence of HLA-B27 cannot be used to tell which disease is present, how quickly it will progress, its severity, prognosis or the degree of organ involvement.
Is there anything else I should know?
Whether or not HLA antigens will be present is genetically determined. Their production is controlled by genes that are passed from parents to children. If one of your family members has a HLA-B27 related disease that affects the joints of the spine (AS or other related condition) and you have the HLA-B27 antigen, then you have a higher risk of developing a similar disease.
With new genetic testing methods, it is now possible to separate HLA-B27 into subtypes. So far, about fifteen different subtypes have been identified. The most common in the U.S. are HLA B27*05 and HLA B27*02. How the presence of these specific subtypes affects the likelihood of developing an autoimmune disease is not yet known.
Common questions
In most cases, the cause is not known. However, in some cases of reactive arthritis, there is an association between a previous infection by a microorganism, such as Chlamydia, Campylobacter, Salmonella, Ureaplasma, or Yersinia, and the onset of the disease. It is thought that similarities between the HLA-B27 antigen and the antigens found on the surface of the microorganisms trigger the immune system to fight both the microorganism and the patient's own tissues, launching the autoimmune disorder after the resolution of the infection.
More information
Pathology Tests Explained (PTEx) is a not-for profit group managed by a consortium of Australasian medical and scientific organisations.
With up-to-date, evidence-based information about pathology tests it is a leading trusted source for consumers.
Information is prepared and reviewed by practising pathologists and scientists and is entirely free of any commercial influence.