

Clotting is a normal part of healing. When you have an injury, and a blood vessel starts to bleed your body triggers a series of chemical interactions to create a blood clot and plug the hole.
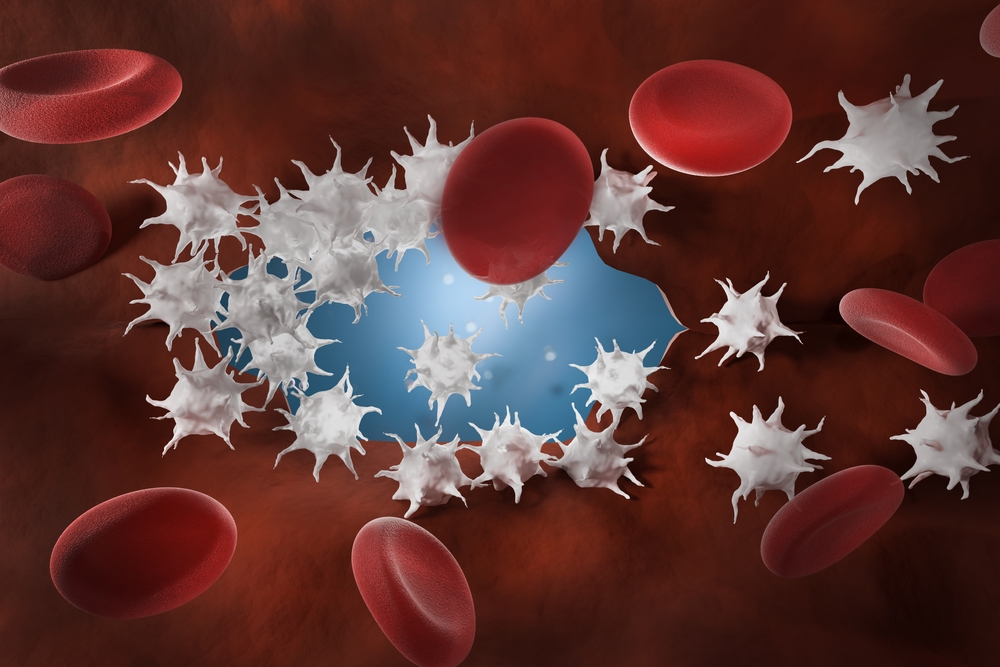
Platelets (thrombocytes) are tiny plate-shaped cells that circulate in your blood. They become activated and travel to the area where they change their shape by growing long tentacles. They become sticky and stick to each other.
When activated, platelets also release chemicals to attract more platelets and other cells, setting off the next step. This is called the coagulation cascade. Substances called clotting factors are activated one after the other, then threads of a protein called fibrin are produced. These threads are glued together to form a fibrin net that catches the sticky platelets and helps hold them together to form a clot.
As the tissue heals and you don't need the clot anymore the fibrin strands dissolve, and your blood takes back the platelets.
If there are too few platelets, or if platelets don’t function properly, there may be problems with blood clot formation. A platelet count is almost always ordered if you have unexplained bruises, or you take an unusually long time to stop bleeding from a small cut or wound. On the other hand, too many platelets can increase the risk of blood clots that can block blood vessels and cause health problems such as deep vein thrombosis, pulmonary embolus, heart attacks or stroke.
Platelets are pieces of very large cells called megakaryocytes. They are made in the bone marrow, the sponge-like tissue inside our bones. Bone marrow contains stem cells that develop into red blood cells, white blood cells, and platelets. New cells are constantly being produced.
Sample.
Blood.
Any preparation?
None
Platelets have a short lifespan in the blood – about five to 10 days. This means the platelet count can rise and fall quickly in response to disease or trauma. Short-term increases in platelet counts are known to be linked to strenuous exercise, childbirth and extreme stress. Platelet counts can vary throughout the course of the day with counts highest at midday.
If an abnormal platelet count is detected then the results of the other blood cells analysed in the FBC, as well as any other tests you have will be considered and further investigations may be requested. This information, along with any clinical symptoms will be used when your medical team makes a diagnosis.
Thrombocytopenia - when you have too few platelets
The normal level of platelets in the blood for an adult is between 150,000 and 400,000 per mL (150-400 x109/L) of blood. (mL = millilitres and L = litres.)
If you have a low number of platelets your condition is called thrombocytopenia. A low platelet count is one less than 150,000 per millilitre (150x109/L) and it can be caused by either of two different processes that reduce the count.
Either the bone marrow is not producing enough platelets, or the bone marrow is producing normal amounts, but the platelets are being used up or destroyed faster than they can be replaced.
| Possible causes of low platelet counts | |
| Immune thrombocytopenia | This is an immune condition that causes platelets to be destroyed faster than they can be replaced. It is one of the most common causes of thrombocytopenia. Diagnosis involves ruling out any other potential cause of a low platelet count. |
| Vitamin B12 or folate deficiency | Severe deficiency of B complex vitamins can lead to anaemia. This is when your body makes red blood cells that are too large and don't work properly. This reduces their ability to carry oxygen. If severe, this can lower your platelet and white cell counts. |
| Drugs and medication | Some medications such as penicillin, gold used to treat arthritis, furosemide, valproic acid and others, can affect platelet production. Heparin (an anticoagulant drug) can cause a sudden fall in platelet numbers in a rare condition called heparin-induced thrombocytopenia (HIT). |
| Infection and viruses | Several infections and viruses can cause a low platelet count. These include parvovirus, cytomegalovirus, and infectious mononucleosis. |
| Liver disease | Liver disease is associated with a low platelet count, among other changes to blood cells and proteins. |
| Autoimmune disorders | Lupus and other autoimmune disorders can cause increased destruction of platelets. |
| Gestational thrombocytopenia | Up to one in 10 women experience a fall in platelet count to below the normal range during pregnancy. If no underlying cause is found, a diagnosis of gestational thrombocytopenia (low platelets caused by pregnancy) is made. |
| Chronic bleeding | Where there is long-term bleeding, such as from a stomach ulcer, platelet counts can be low. |
| Leukaemia or lymphoma | Cancers of the white blood cells affect the function of the bone marrow and platelet numbers will be reduced. |
| Rare inherited platelet disorders | These include Bernard-Soulier syndrome, Glanzmann Thrombasthenia and MYH9-related thrombocytopenias and are associated with a reduction in circulating platelets together with an increased platelet size (giant platelets). |
| Bone marrow disorders/invasion | Diseases affecting the bone marrow such as myelodysplasia, aplastic anaemia, or other haematological conditions, or invasion of the bone marrow by other cancer cells (metastasis) can affect platelet production. |
| Chemotherapy and radiotherapy | Chemotherapy and/or radiotherapy will affect the function of the bone marrow and result in reduced production of all blood cells, including platelets. |
| Systemic disorders | Some serious disorders can result in multiple abnormalities of blood cell counts and characteristics. These include haemolytic uraemic syndrome (HUS), and thrombotic thrombocytopenic purpura. |
| (TTP) and disseminated intravascular coagulation (DIC) | These are examples of syndromes in which someone will have reduced platelet counts alongside other clinical symptoms and blood cell changes. |
Thrombocytosis – when you have too many platelets
A high platelet count of more than 450,000 per millilitre (450x109/L) is called thrombocytosis and is due to either:
| Secondary thrombocytosis - possible causes of high platelet counts | |
| Infection | The platelet count may be increased in response to many infections. |
| Inflammation | Chronic conditions such as Crohn’s disease, or other inflammatory processes can increase the platelet count. |
| Recent trauma | Platelet counts can rise due to tissue damage, or after a surgical operation. |
| Poor spleen function | People who have poor spleen function or who have had their spleen removed can expect raised platelet levels. |
| Bleeding or recent blood loss | Platelet counts go up in response to bleeding. |
| Iron deficiency anaemia | This is particularly the case when the anaemia is due to chronic blood loss such as from a stomach ulcer. |
| Cancer | High platelet counts are commonly found in association with lung, breast and ovarian cancer. |
| Drugs/medication | Medications such as corticosteroids can stimulate platelet production. |
| Rebound phenomenon | Platelet counts can rise after treatment with growth factors or during recovery following chemotherapy. |
Bone Marrow disorders and myeloproliferative neoplasms/ myeloproliferative syndromes
Primary or essential thrombocythaemia (ET) and polycythaemia vera (PV) are disorders in which too many platelets are produced in the bone marrow in an uncontrolled way.
These conditions might not cause any symptoms and are often picked up incidentally when a full blood count is performed as a routine check or for another reason.
Although in some people there may be no clinical signs or symptoms, there are risks associated with having abnormally high platelet counts, including blood clots and risk of bleeding.
PV is associated with mutations (variants) in the gene JAK2. ET is associated with mutations in the JAK2, MPL or CALR genes. If PV or ET is suspected, then tests to look for variants in these genes may be carried out.
Different types of bone marrow disorders such as chronic myeloid leukaemia (CML), myelodysplasia (MDS) and other myeloproliferative syndromes can also be linked to high platelet counts.
Reference Intervals
The results of each component will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation and your results need to be interpreted by your doctor.
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record.
You and your healthcare provider can now access your results whenever and wherever needed. Get further trustworthy health information and advice from healthdirect.