

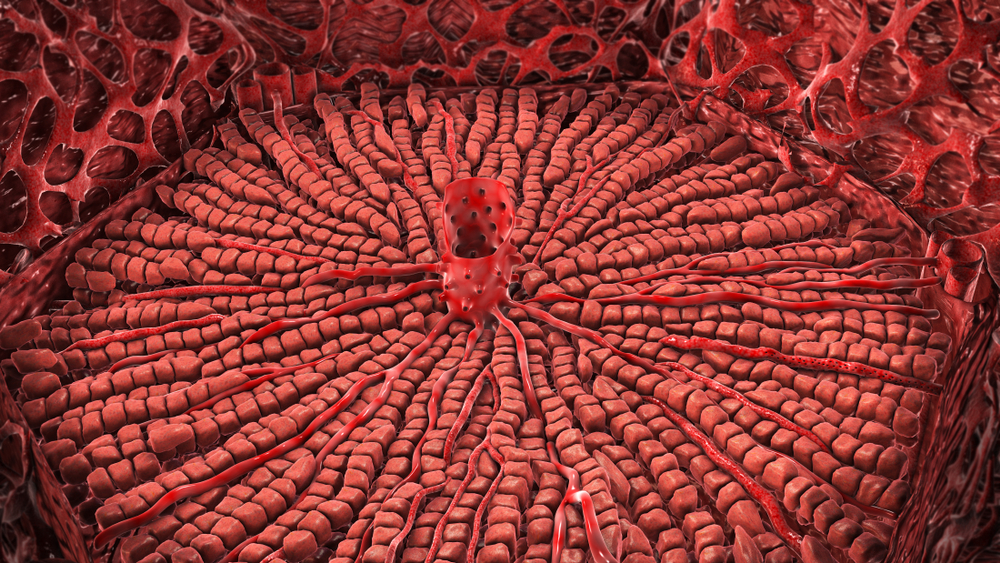
The liver is one of the most important organs in the body. It has an essential role in digesting food and removing harmful substances from the blood. It breaks down nutrients and chemicals in the blood into forms that are easier for your body to use. It breaks down and removes drugs and substances that could be harmful. It also produces bile, which is a fluid that helps break down fats making it easier for digestive enzymes to process and absorb them. It also removes waste products from your body.
The liver also produces blood clotting factors, it controls the amount of blood in your body and stores vitamins and glycogen for energy. Importantly, the liver is a key component of the immune system removing potentially harmful bacteria and viruses from the body.
What causes liver damage?
Many diseases can damage your liver but most liver disease is due to lifestyle factors such as alcohol, being overweight or obese and infections, especially viral hepatitis. Together alcohol, excess bodyweight and viral hepatitis are the cause of nine out of 10 cases of liver disease.
As liver disease progresses, the liver becomes inflamed which causes scarring and stiffening. It can become quite damaged before symptoms appear. In the early stages, there are often no symptoms or else mild non-specific symptoms, such as tiredness and nausea. As liver disease progresses and it causes inflammation, your bile duct can become blocked, and you may experience blood clotting problems.
In the early stages, scarring can be reversed. The liver is the only internal organ that can regrow itself and treatment and/or lifestyle changes can give the liver the time it needs to heal. Eventually, there is so much scarring that it cannot be reversed, your liver cannot work properly, and this increases the chance of liver failure, a life-threatening condition. This is known as liver cirrhosis.
Acute and Chronic Hepatitis
| Hepatitis is a term used for inflammation of the liver. It can be either acute or chronic. | |
| Acute Hepatitis | This is fast-developing and typically makes you feel ill with loss of appetite and sometimes diarrhoea and vomiting. In many cases, acute hepatitis causes jaundice - when your urine turns brown, and skin and eyes become yellow. It is usually short-lived and resolves in a few months. Acute hepatitis can be caused by drugs, alcohol, some conditions involving your immune system, and any condition that blocks the release of bile from the liver. Hepatitis A virus is the most common cause of acute hepatitis. Liver diseases that are due to the changes in your body during pregnancy can cause acute hepatitis. |
| Chronic Hepatitis | This is when liver inflammation lasts longer than six months. It usually causes no symptoms or only a loss of energy and tiredness. Most people don’t know that they have it. Chronic hepatitis can gradually damage the liver and, after many years, cause it to fail. Chronic hepatitis is usually caused by hepatitis B or C infection, alcoholic liver disease and/or fatty liver. |
Your medical team may order LFTs:
You may also have other blood tests to assess your general health such as:
More specific tests may be needed to check for viral infections especially hepatitis A, B, or C or the antibodies that are known to be linked to autoimmune liver disease. There are several forms of autoimmune liver disease.
Inherited conditions can cause severe liver disease. If haemochromatosis is suspected, your medical team may request a full blood count (FBC), which gives information on the amount of haemoglobin in your blood, as well as the size and shape of the red blood cells, and iron studies, a group of tests that looks at the overall iron status in your body. If your results suggest haemochromatosis, an HFE genetic test may be ordered to make a definitive diagnosis.
If your medical team considers you may have an inherited condition called Wilson’s disease, the copper levels in your blood may be measured. It is important to tell your doctor of any family history of liver problems. Early detection of these conditions allows them to be treated and managed appropriately.
Imaging tests that can show liver damage include ultrasound, CT (computerized tomography) and MRI (Magnetic resonance imaging) scans. A liver biopsy maybe done to help confirm a diagnosis and assess the extent of liver damage.
Sample
Blood.
Any preparation?
None.
Your LFT results cannot diagnose a specific disorder and can only show that your liver may not be working as it should. Each of the LFTs gives different information about your liver function and the combined results can indicate patterns usually seen with particular types of liver disease or damage. The changes in the different substances will help your doctor decide what could be wrong with your liver, and what further tests may be needed to confirm the type of liver disease you may have.
| Liver Function Tests - Components | |
| Alanine aminotransferase (ALT) | ALT is an enzyme found mostly in the liver. Smaller amounts are also found in the kidneys, heart and muscles. Normally, ALT levels are low but when the liver cells are damaged, they release ALT into the bloodstream. This usually occurs before more obvious symptoms of liver damage can be seen. A very high level of ALT is often seen with acute hepatitis. Moderate increases may be seen with chronic hepatitis. People with blocked bile ducts, cirrhosis, and liver cancer may have ALT levels that are only moderately raised or close to normal. |
| Alkaline phosphatase (ALP) | ALP is an enzyme found throughout your body. It allows certain bodily processes to happen. The two main sources of ALP in your blood are your liver and bones. High levels of ALP may indicate liver disease or certain bone disorders. ALP may be significantly increased when there are obstructed bile ducts, liver cancer, and with bone disease. Raised levels of both ALP and GGT indicate liver disease rather than bone disease. |
| Gamma- glutamyl transferase (GGT) | GGT is an enzyme found mainly in the liver and is normally present in low levels in the blood. When the liver is damaged or the flow of bile is obstructed, GGT level rises. It is therefore a useful marker for detecting bile duct problems. A GGT test may be used to help decide the cause of a raised ALP. Both ALP and GGT are raised in bile duct and liver disease, but only ALP will be raised in bone disease. Increased GGT levels are also seen with alcohol overuse and often in people taking drugs that are metabolised in the liver such as carbamazepine and phenobarbitone. |
| Aspartate aminotransferase (AST) | AST is an enzyme which is mostly in the liver but also in red blood cells, heart and other muscles. When liver, red blood cells, heart or muscle cells are injured they release AST into the blood. A very high level of AST is often seen with acute hepatitis. AST may be normal to moderately increased with chronic hepatitis. In people with blocked bile ducts, cirrhosis, and liver cancer, AST concentrations may be moderately increased or close to normal. When liver damage is due to alcohol, AST often increases much more than ALT (this is a pattern seen with few other liver diseases). AST is also increased after heart attacks and with muscle injury. |
| Bilirubin | Bilirubin is a yellowish pigment that is made during the body's normal process of breaking down old red blood cells. It is processed by the liver to be removed from the body. If your liver is healthy only small amounts of bilirubin are found in blood but if your liver isn't working properly bilirubin levels rise. Bilirubin is increased in the blood when too much is being produced or too little is being removed, due to bile duct obstructions, or to problems with bilirubin processing. High levels of bilirubin are responsible for jaundice – when your skin and the whites of your eyes become yellow. It is not uncommon to see high bilirubin levels in newborns, typically under three days old. |
| Albumin | Albumin is the main protein made by the liver and helps carry hormones, vitamins, drugs and minerals such as calcium through the bloodstream. One of its most important roles is helping to maintain fluid balance in the body by preventing fluid leaking from the blood vessels into other tissues. People who have chronic liver disease and kidney disorders are at risk of developing low albumin levels. This is due to decreased production in the liver or too much being lost through damaged kidneys. Without enough albumin fluid can build up in your lungs and other parts of your body. Although levels can be normal in early-stage liver disease as damage worsens the liver is less able to produce enough albumin. Measuring albumin can check for the severity of liver disease. |
| Total Protein | The total protein test measures albumin and all other proteins in blood, including antibodies. Total protein levels are often normal with liver disease. |
| Prothrombin Time (PT) | Prothrombin is a protein that acts as a clotting factor in your blood. It is an important factor in your blood that help it to clot and prevent excessive bleeding. It made by the liver. A prothrombin time (PT) test measures how long it takes for your blood to clot. If the test shows that your blood takes longer to clot than it should, it can be a sign of liver disease. |
Reading your test report
Your results will be presented along with those of your other tests on the same form. You will see separate columns or lines for each of these tests.
Results of LFTs are usually assessed together. Several sets of results from tests performed over a few days or weeks are often assessed together to see if there is a pattern. Your test results will typically change over time.
It is possible to have abnormal results but not have liver disease. Many temporary conditions, such as shock, burns, severe infections, muscle trauma, dehydration, pancreatitis, haemolysis, and pregnancy can cause one or more of the liver function tests to be abnormal.
If you are taking medication that may affect your liver, abnormal test results may indicate a need to re-evaluate the dosage or choice of medication.
LFTs are helpful in monitoring the effectiveness of any treatment you have, or lifestyle changes you make.
Reference Intervals
Your results will be compared to reference intervals (sometimes called a normal range).
If your results are flagged as high or low this does not necessarily mean that anything is wrong. It depends on your personal situation. Your results need to be interpreted by your doctor.
The reference intervals for all LFT's except GGT have common reference intervals which means that all laboratories in Australia should be using the same ranges for these tests.
The choice of tests your doctor makes will be based on your medical history and symptoms. It is important that you tell them everything you think might help.
You play a central role in making sure your test results are accurate. Do everything you can to make sure the information you provide is correct and follow instructions closely.
Talk to your doctor about any medications you are taking. Find out if you need to fast or stop any particular foods or supplements. These may affect your results. Ask:
Pathology and diagnostic imaging reports can be added to your My Health Record.
You and your healthcare provider can now access your results whenever and wherever needed. Get further trustworthy health information and advice from healthdirect.